A Spotlight PA/KHN investigation shows the Department of Drug and Alcohol Programs uses an inherently flawed oversight system that does little to ensure high-quality or effective care.
Aneri Pattani of KHN and Ed Mahon of Spotlight PA
This investigation is a joint project of KHN, a national newsroom that produces in-depth journalism about health issues, and Spotlight PA, an independent, collaborative newsroom dedicated to producing investigative journalism for all of Pennsylvania.
When Ian Kalinowski was at work, his mom usually texted him. So when he saw her number show up as an incoming call around lunchtime one Tuesday, he figured it had to be important.
Now, more than seven years later, he remembers her screams, the shock, and the questions she asked over and over again.
“Why are they saying this to me? Why are they lying to me?” Ian recalled his mom asking. “They’re telling me Adam’s dead. Why would they do this to me?”
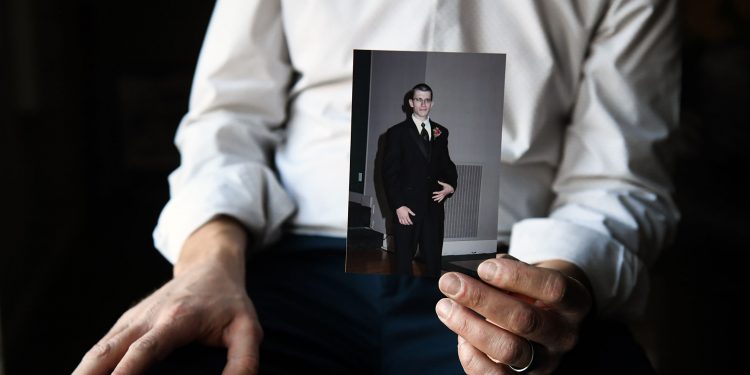
Adam was Ian’s older brother. Growing up, it seemed they spent every second together. Football, hockey, and tag filled long days outside their Pittsburgh home. When Ian moved away for college, he and Adam turned to online poker to stay in touch. Adam served as best man at Ian’s wedding, and Ian admired his brother’s artistic streak. Adam could turn any piece of paper into an origami swan. His mom’s home is still full of swans.
Adam’s struggle with opioid and alcohol addiction was painful for Ian to watch. The problems began, it seemed to Ian, after Adam dropped out of college and used drugs to deal with his depression. Adam sought treatment, and he relied on methadone for many years, but his problems continued. When he was 32, he typically drank dozens of beers each day. On Feb. 3, 2014, he entered a treatment center run by Addiction Specialists Inc., according to a lawsuit later filed by his family against the facility. The center, in a Fayette County strip mall, was about an hour’s drive south of Pittsburgh.
Less than 24 hours after Adam made it to the facility, he was dead, according to expert reports from doctors in the family’s wrongful death lawsuit. Ian couldn’t understand what went wrong, and neither could his mom, still in denial on the other end of the phone call.
What his family didn’t know was that Addiction Specialists Inc., often known as ASI, had a history of violating state rules. In a later federal investigation into the facility’s billing and drug distribution practices, a grand jury concluded that a litany of problems occurred at the business many months before and after Adam’s arrival.
In the wrongful death suit, a lawyer for the Kalinowski family alleged Adam wasn’t evaluated by a physician when he arrived at ASI, didn’t receive the medication or treatment he needed, became increasingly uneasy and anxious throughout the night, and killed himself. An Allegheny County judge in December 2019 said the business, two of its owners — Rosalind and Sean Sugarmann — and an ASI physician were negligent in caring for Adam. The judge ordered them to pay over $1.6 million in damages, although Ian doubts they ever will.
ASI eventually shut down, two years after Adam died.
In recent interviews with Spotlight PA/KHN, the Sugarmanns denied responsibility for Adam’s death and maintained that ASI was a good facility. Rosalind said it helped a lot of people in a rural area with a high drug-overdose rate.
Addiction treatment facilities in Pennsylvania, like ASI, are licensed and regulated by the state to ensure they follow certain rules and keep vulnerable people struggling with addiction safe. Oversight used to fall to the Department of Health. But in 2012, the state created the Department of Drug and Alcohol Programs, a $125 million agency set up to give substance use the attention lawmakers felt it deserved.
At the time of Adam’s death in 2014, the department had taken few disciplinary actions against ASI. It had issued citations and required the company to submit plans to correct them. But the Sugarmanns told Spotlight PA/KHN that, at the time, they didn’t fear the state would shut them down.

Perhaps for good reason.
A Spotlight PA/KHN investigation found that the department has allowed providers to continue operating despite repeated violations of state regulations and harm to clients. More than 80 interviews and a review of thousands of pages of state government and court records revealed that the department lacks resources and regulatory power, uses an inherently flawed oversight system that does little to ensure high-quality or effective care, and rarely takes strong disciplinary action against facilities when so many Pennsylvanians need services.
The department has no standard criteria for when it should force facilities to serve fewer patients and, as of early April, had revoked just one treatment provider’s license in nearly a decade. It doesn’t, as a regular practice, compare facilities to see if any stand out for an unusual number of violations or the most client deaths. And since state inspections focus heavily on records, they can be tricked with fraudulent paperwork, former employees in the treatment field said.
This leaves Pennsylvanians — who suffer one of the highest drug overdose death rates in the nation — in the dark about which treatment facilities have troubling track records.
Some advocates point out that overregulating or closing facilities could leave people suffering from addiction without options for care. But in the current system, state and judicial records show, some patients have received inadequate treatment or even died; certain facilities have fraudulently billed insurance companies; and owners rake in federal and state tax dollars, as well as private money from victims of the opioid crisis.
“Many of these rehab facilities are not properly run or supervised, and many are in it for the money,” said Peter Friday, an attorney who represented Adam’s family in their lawsuit. “These places have been unbridled.”

Who polices the providers?
Even though the Department of Drug and Alcohol Programs provides the licenses that allow addiction treatment facilities to operate, Jennifer Smith, secretary of the department, said it has limited responsibility for them. Law enforcement agencies are often better positioned to take action against troubled providers, she said, and insurance companies that pay for services also offer oversight.
“It’s not our job to really police the providers,” Smith said in an interview. “Our function is to really try to enable them to meet the [state’s] requirements, and by doing so, enabling them to provide quality services.”
Yet, as the regulating body of these treatment facilities, the department collects some of the most critical information necessary to properly police them, including reports of client deaths and physical and sexual assaults.
Smith said most providers are trying to do good work. She said annual inspections ensure facilities meet safety standards, like having enough staff members and a building that’s up to code. But inspections are not meant to evaluate quality of care, she said.
The Spotlight PA/KHN investigation found the department makes little of what it knows about troubling facilities accessible to the public. Its website shows if a facility currently has a provisional license — a designation indicating the provider failed to meet several state requirements and will be inspected more frequently until it resolves those concerns — but not whether it ever received such a sanction in the past, for what issues, nor how they were resolved.
The department does not post the reports it collects about deaths and assaults, which represent some of the most concerning events at treatment facilities.
When Spotlight PA/KHN filed a public records request for those reports, the department shared only incidents that it decided did not warrant investigation. It said it could not provide the total number of such events at specific facilities since it doesn’t have aggregate data prior to September 2019, when it launched a new electronic reporting system. Even the available data from that new system provides an incomplete picture, as less than a quarter of treatment facilities had enrolled in the voluntary system as of March 2021.
Smith said people should pick facilities the same way they do primary care doctors, based on publicly available information, personal recommendations, and discussions with insurers.
One of the main public resources the department offers is a website with reports from its facility inspections. Inspectors write these reports after a site visit, listing any violations of state regulations they found. But these reports provide a limited window into the daily reality for clients, as there’s no indication of which violations are more severe than others, and many regulations focus on building conditions and completion of records. One regulation, for example, mandates the temperature at which refrigerated food must be maintained.
In response to each violation inspectors find, the facility submits a plan to address it. If the facility fails to provide a plan or follow through on it, the department has two primary options: force the facility to reduce the number of clients it serves or issue a provisional license. If the department wants to permanently revoke a facility’s license, it must go through an administrative court process to get approval.
In nearly a decade before December 2020, the state issued provisional licenses to fewer than 80 facilities — less than 10% of providers — and forced only three to reduce their capacity, according to data from the department. In ASI’s case, regulators said multiple times that the company failed to document that it provided required counseling and other services. A department spokesperson said it didn’t force ASI to operate under provisional licenses before 2015 because the business submitted plans of correction the department found acceptable. Even if a facility has many violations, the department considers how cooperative it is in working to fix them, Smith said.
After a recent reorganization, the department formed a quality improvement unit with three employees, Smith said. The unit may work directly with treatment facilities but is meant to address broader prevention efforts and other addiction-related programs as well. The department is also working with a national company to provide an online platform where clients can leave reviews of facilities, starting in spring 2022.
But many employees and clients in the treatment field are skeptical of any long-term improvement. For years, they’ve seen troubled facilities make fixes, only to have the same deficiencies arise in later inspections.
The department’s own records show the cycle can persist for years.

Years of citations, little action
At SOAR Corp methadone clinic in Northeast Philadelphia, inspectors from the state Department of Health first issued citations for unqualified employees in 2009, before the Department of Drug and Alcohol Programs was created and took over inspections in 2012. Inspectors at the time also found one counselor who was responsible for 40 clients — above the state-mandated maximum of 35.
SOAR Corp responded by saying it had demoted an unqualified counselor, had hired another counselor to lower caseloads, and would ensure future hires met the state’s requirements.
But state records show that within a year of those 2009 citations, the facility was cited three more times for similar issues: hiring an unqualified project director, overloading counselor caseloads, and lacking enough medical personnel. Year after year, state inspectors found the same problems. Yet the state approved SOAR to open additional locations in Lansdowne, Levittown, and Warminster in 2010, 2016, and 2018, respectively.
In interviews with Spotlight PA/KHN, a dozen former employees and nearly a dozen current and former clients across multiple SOAR sites complained about poor hiring practices and chronic understaffing as just two symptoms of their much larger concerns. They believed the company relentlessly pursued profits by getting as many clients in the door as possible, with little care for the quality of treatment.
The Philadelphia location has received three provisional licenses from the state, in 2012, 2019, and 2020, putting it among the 10 most frequent recipients of this sanction over nearly the past decade.
The former counselors felt that expectations to maximize “billable hours” led to their burnout. And they saw high turnover among staffers. The former and current clients said they sometimes went weeks without therapy or were switched from one overwhelmed counselor to another every few months.
Nicole Tihansky was a client at SOAR’s Levittown location for about a year until last fall. She said she waited more than a month before getting her first counseling session, and then was assigned about five counselors, one after the other.
“It makes you just want to get in and out of the session quickly, because you know you’ll get another counselor in a month,” she said.
Understaffing is a problem across the treatment industry, according to employees in the field. But former SOAR employees who have worked for multiple companies said SOAR stood out in their experiences for its high staff turnover and inadequate therapy.
“It’s not about therapy or addressing the needs of clients,” said Esther Kirshenbaum, a counselor who worked at the Philadelphia location from 2017 to 2019. “The attitude is to just get clients in here and make sure we get paid.”
In a statement, SOAR CEO Richard Mangano said the company “makes every effort to comply with local, State, and Federal regulations.”
Spotlight PA/KHN shared with SOAR a detailed list of more than a dozen allegations from their reporting, including violations of state regulations and putting profits over patient care. Mangano did not address them specifically.
“Soar Corp categorically denies any allegation or suggestion of wrongdoing. … Soar Corp has and will continue to work with DDAP to improve the important services it provides,” Mangano wrote, referring to the Department of Drug and Alcohol Programs.
In its responses to state citations in recent years, SOAR explained that clients didn’t show up to scheduled counseling sessions, and that services like drug tests and physician evaluations had been provided but simply not documented properly.
The Department of Drug and Alcohol Programs has never forced SOAR to decrease its capacity, nor have state officials initiated the administrative court process to permanently revoke its license.
Former clients and employees said state licensing inspections were announced ahead of time, causing a rush by SOAR employees in the days before a site visit to complete treatment plans, counseling notes, and other required paperwork.
Nicholas Cucchiaro was a SOAR counselor from 2017 to 2018. He shared with Spotlight PA/KHN what he reported to the Department of Drug and Alcohol Programs and the Pennsylvania Office of Attorney General after he was fired. He told the agencies that a senior administrator at SOAR instructed him to make up counseling notes for clients who had gone weeks without an assigned therapist.
“These are notes from therapy sessions that never happened,” he said, adding he knew it was wrong but feared losing his job if he didn’t comply.
About a dozen other former employees and clients described to Spotlight PA/KHN their own experiences of similar practices, ranging from thrusting months’ worth of forms upon clients in the days before an inspection to backdating their paperwork.
The Department of Drug and Alcohol Programs and the attorney general’s office both agreed to look into the allegations, Cucchiaro said, but he didn’t hear of any consequences for SOAR.
The attorney general’s office told Spotlight PA/KHN that it reviewed “a small number” of complaints regarding SOAR and referred the matter to the Department of Drug and Alcohol Programs.
Smith, the department head, said that as a general matter it’s difficult to prevent facilities from falsifying paperwork, because state regulations require advance notice of licensing inspections. But if the department receives a complaint, it can conduct unannounced inspections, she said, and other facilities have been cited for fraudulent paperwork.
Unannounced site visits were made in response to the complaints at SOAR, according to a department spokesperson, and citations were issued for violations that did not include fraudulent paperwork. SOAR’s Philadelphia location received provisional licenses in 2019 and 2020, but as of mid-April all the company’s sites were operating on full licenses after remedying the cited issues.
A growing industry
One significant limitation on the department’s oversight is its inability to impose financial penalties on treatment facilities.
In contrast, the state’s environmental protection and health departments can fine polluters and nursing homes for violations.
A 2017 report from the state auditor general’s office urged lawmakers to allow the department to charge licensing fees and assess financial penalties, pointing to other states that do so. Smith told Spotlight PA/KHN that fining facilities would help weed out repeat violators.
A bill introduced in the Pennsylvania legislature to allow the department to generate licensing fees went nowhere two years ago. A similar measure was recently referred to the state Senate Health and Human Services Committee.
“I hope that it’s considered quickly as ensuring drug treatment facilities are given appropriate oversight is of utmost importance,” the bill’s sponsor, state Sen. Judy Schwank (D., Berks), said in a statement.
Meanwhile, with millions of dollars on the line, the treatment industry is growing in Pennsylvania. Over the last four years, the state has seen a net gain of about 40 facilities, the department said, bringing the total to more than 800 treatment providers. State budget documents suggest the industry’s client capacity has grown by about 5,000 over a similar period.
The Department of Drug and Alcohol Programs employed 82 people, including two dozen who conduct facility inspections, as of April. That’s about half the number of dog wardens employed by the state to inspect kennels.
Smith said there is “adequate staff to perform our current licensing responsibilities.”
In December 2018 — the same year the department said it received complaints from former SOAR employees and clients — it approved the company to open a location in Warminster. Inspection surveys at the facility since have found it violated state rules by providing a certain medication without state approval and failing to provide the required hours of therapy to some patients.
A former SOAR supervisor who is still working in the treatment industry and asked not to be named doubts the state will ever take stronger action against the company.
“The state knows the demand for treatment and the demand for medication-assisted treatment,” the former supervisor said. “If you took SOAR’s license in Northeast Philadelphia and didn’t give them a provisional, you could be displacing 500 clients.”
The need for treatment
The urgency of the opioid crisis puts regulators in a tough position: If they shut down a facility, where will all the patients get treatment?
James McKay, a professor at the University of Pennsylvania’s medical school who researches the efficacy of addiction treatments, said facilities that are committing insurance fraud or actively harming patients should be penalized. But the question becomes more complicated when judging how well a facility is serving its clients.
In Philadelphia, where there are many treatment programs, it might make sense to close one that has ineffective interventions, untrained counselors, and many clients dropping out, McKay said.
“But if you’re out in the middle of the state and there’s only one treatment program in any reasonable distance, as long as they’re not treating you badly, you’re at least going to get some support and meet others in recovery,” he said. “So much of this depends on what the other alternatives are.”
In Western Pennsylvania, an inpatient detox and rehab facility called Clear Day Treatment of Westmoreland has received multiple provisional licenses since it opened in 2018. State inspectors have noted at least six incidents that involved drugs on the premises and have cited the facility at least twice for understaffing, writing that the lack of sufficient staff fails to ensure “efficient and safe operation.”
Despite these concerns, the facility is the only one in the county that provides detox services while allowing patients to stay on any of three medications for opioid use disorder. Many patients in the area need that service, said Colleen Hughes, executive director of the Westmoreland Drug and Alcohol Commission Inc. (The commission is one of more than 40 agencies across the state that the Department of Drug and Alcohol Programs contracts with to coordinate substance use services locally.)
The commission determined in 2017 that a lack of residential rehabs in the county was one factor delaying people’s treatment. Clear Day responded to a request for proposals to meet that need from companies that manage Medicaid-paid behavioral health for the state in that region. Clear Day has been awarded nearly $750,000 in state Medicaid funds left over from previous years to help with start-up costs, according to Southwest Behavioral Health Management, Inc., one of the companies that put out the request.
Stephen Devlin, executive director of Clear Day, said in a statement that Southwest Behavioral Health Management closely monitored those funds, which helped the facility provide “much needed” addiction treatment services.
“State auditors have been diligent in ensuring that Clear Day addressed all deficiencies that have been identified during audits,” Devlin wrote, “and, further, that Clear Day provides strong and effective treatment to the individuals in our care.”
Hughes said her office has addressed the issues of understaffing and drugs on the premises with Clear Day through meetings and training sessions.
Smith, head of the Department of Drug and Alcohol Programs, said: “None of us want to see providers closing. We want them to be successful. We want them to be able to deliver the services for their benefit and for ours.”

Waiting for consequences
In Fayette County, ASI came under fire from state and federal authorities in 2015.
The FBI raided the facility that October. The following January, a federal grand jury indicted one of the owners, Rosalind Sugarmann, and an ASI doctor on multiple counts of illegally distributing a medication to treat opioid addiction.
Nearly three months later, a counselor employed by ASI overdosed while staying at the facility, an attorney for the state later said in an administrative court filing against ASI. Ultimately, a bankruptcy case forced the business to close.
In late 2016, Sugarmann pleaded guilty to illegal drug distribution and health care fraud. But that hasn’t kept her and her family out of the recovery business. Less than a year after she was released from prison, Sugarmann — who has talked publicly about her own substance use decades ago — announced she was opening a recovery home.
“I’m not going to stop working with addicts ever. That’s my calling in life,” Sugarmann said in an interview with Spotlight PA/KHN. “Somebody helped me, and I help somebody else.”
But two families said Sugarmann failed their loved ones.
There’s Adam Kalinowski, who died at ASI in 2014, and there’s 37-year-old James Pschirer, who died of an overdose in a recovery home Sugarmann’s family operates. These homes offer peer support and often have curfews and rules designed to help people stay away from drugs after they’ve been discharged from inpatient treatment.
In Kalinowski’s case, Sugarmann said ASI reported his death to everyone it was required to. There’s no indication from department records that the state cited ASI in connection with his suicide.
(The Department of Drug and Alcohol Programs wouldn’t comment on Kalinowski’s case specifically but said it worked with the FBI to investigate problems at ASI.)
Neither Sugarmann nor her husband, Sean, mounted a defense against the Kalinowski family’s lawsuit in court. In a recent interview with Spotlight PA/KHN, Sean Sugarmann placed the blame for Kalinowski’s death elsewhere, saying that the facility was staffed correctly and that, given his eventual suicide, Kalinowski never should have been sent to ASI.
Kalinowski’s family also sued UPMC Mercy, the Pittsburgh hospital where he was treated before going to ASI, and affiliated entities, but resolved the claims against them through a private settlement, according to a family attorney. UPMC denied responsibility for Kalinowski’s death. In a pretrial court filing, an expert witness for UPMC directed blame at ASI, saying Kalinowski was well enough to be safely discharged to a residential treatment facility. That he wasn’t evaluated by a doctor, nurse, or professional counselor when he arrived at ASI was a concern, the expert wrote, and “perhaps this tragedy could have been avoided” if ASI had provided a higher level of care.
More recently, Rosalind Sugarmann has faced criticism for her involvement with recovery homes.

In February 2019, while still under federal supervision, Sugarmann announced on a blog that she was “back in commission!!” and would open a men’s recovery home called The Second Act outside Pittsburgh.
A 2017 law gave the Department of Drug and Alcohol Programs new power to regulate recovery homes in addition to treatment facilities. The state missed a June 2020 deadline to implement the voluntary licensing process but plans to roll out the program this year.
James Pschirer turned to The Second Act for a place to stay in the fall of 2019. His mother, Andrea Zack, helped him with rent, writing out a $250 check to Sugarmann, according to a photocopy of the check the family provided.
Then, on Nov. 1, 2019, James died inside the home from a fentanyl and cocaine overdose, a photo of the death certificate provided by his family showed.
Andrea and James’ sister, Amanda Pschirer, went to The Second Act to collect his clothes and personal items. Andrea kept the coins in his pockets, knowing he had touched them.
It wasn’t until after James’ death that his family found out about Sugarmann’s criminal conviction, they said.
Amanda knows her brother chose to use drugs, but she thinks he could still be alive if he had stayed in another home with better oversight. And she’s angry that nothing stopped Sugarmann from being involved with one.
“I am worried that someone else will die under her care,” Amanda said.
In interviews, Rosalind and Sean Sugarmann downplayed their involvement with The Second Act. “My kids are involved in the recovery homes,” Rosalind told Spotlight PA/KHN. “I’m not an owner there.” The business is registered in their children’s names, and Rosalind said she’s lived in Los Angeles since early 2020.
Still, Sean Sugarmann acknowledged helping his adult children manage the business, and said in March he was living in the men’s home at that time. One of his daughters referred questions about The Second Act to Sean. Rosalind promotes the business on social media accounts, encouraging people to move in. She told Spotlight PA/KHN, “I’m not gonna deny that I’m a consultant.”
Sean said an overdose death “could have happened anywhere, and I think it happens everywhere.”
Last fall, Amanda Pschirer reached out to state officials with concerns about recovery homes. But she said she didn’t receive a response for four months. The department said a computer glitch with an online form, discovered in January, caused the delay in responding to her submission and about 260 others.
Ian Kalinowski, whose brother died at ASI seven years ago, has followed Rosalind’s posts online and saw that she’s still involved in the recovery business. He’s outraged.
He and his family are still grieving Adam’s loss. Ian wishes his young children had gotten to meet their uncle. He doubts the ASI defendants will ever provide the $1.6 million-plus that the judge said they owe.
Ian recognizes that ASI’s leaders faced some consequences for problems at the business.
“But there have still been no repercussions for what happened to my brother,” he said of the Sugarmanns.
He’s not optimistic there ever will be.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Spotlight PA is powered by The Philadelphia Inquirer in partnership with PennLive/The Patriot-News, TribLIVE/Pittsburgh Tribune-Review, and WITF Public Media. The independent, nonpartisan newsroom is funded by foundations and readers like you who are committed to accountability journalism that gets results: spotlightpa.org/donate.