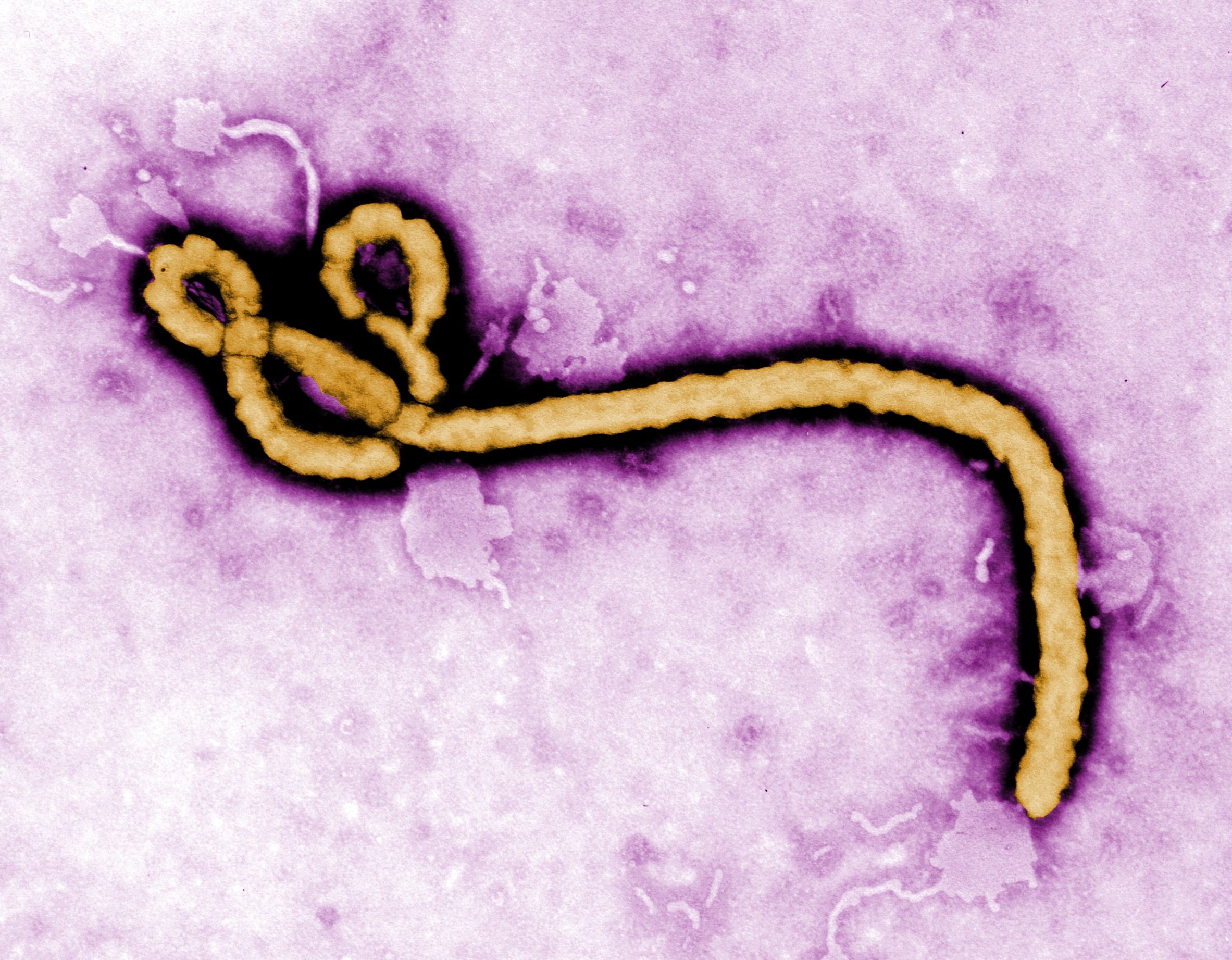
Despite a massive international effort, several treatments that once held great hope for fighting Ebola have turned out not to work against the dreaded virus that killed more than 11,000 people.
The “harvest of that massive effort is thin,” writers in the journal, Science, recently commented.
But researchers are looking into some other options, with more studies coming out just in the past week. Here’s where various Ebola treatments stand, both the losers and those still up for consideration.
What’s not working
Studies show these three treatments don’t seem to work:
Blood donations from Ebola survivor
Infusing an Ebola patient with blood products from an Ebola survivor was a treatment that met with great fanfare and publicity in the United States. Dr. Kent Brantley, the first American Ebola patient, received a transfusion from a Liberian boy, and then donated his own plasma to at least four others: fellow charity worker Dr. Rick Sacra, Dallas nurses Nina Pham and Amber Vinson, and NBC videographer Ashoka Mukpo. Another charity worker, Nancy Writebol, donated her plasma to Dr. Craig Spencer in New York City.
A study in last week’s New England Journal of Medicine, which looked at 84 patients who received plasma donations, found it didn’t help save lives.
American doctors treating patients in the U.S. all said they could not attribute the recovery of their patients to a single or combination of treatments, and would never know what worked. That several Americans survived after receiving plasma is generally chalked up to the fact that their disease was caught early and they were kept well hydrated, a key factor in surviving Ebola.
Brincidofovir
Mukpo, the NBC camerman, was given Brincidofovir. The experimental drug has worked for some patients with various viral infections, but a study on brincidofovir and Ebola ended abruptly last year.
Chimerix, the U.S. company that makes it, withdrew its drug from the trial without clearly explaining why, according to Martin Friede, who leads the World Health Organization’s coordination of Ebola treatment research.
The cancellation of the much-heralded study was “embarrassing,” Friede said. But he added that it taught the research world a lesson: Don’t start studies with human beings based on thin evidence that the drug might work. “The trials were started based on a single piece of data, and one piece of data isn’t sufficient,” he said.
TKM-Ebola
Sacra, the doctor who does charity work in West Africa, received this experimental drug in 2014, but a study was halted last year when it became clear the drug didn’t help people with Ebola, Friede said.
The Canadian company that made TKM-Ebola changed its name from Tekmira to Arbutus and switched its focus away from Ebola and toward hepatitis B.
Reasons for hope
Experts are cautiously optimistic that one of these three drugs might be an effective treatment for Ebola:
Zmapp
When asked to name the leading candidate drugs to fight Ebola, Friede with the WHO has a swift answer: “There’s only one real leading candidate, and that’s Zmapp.”
Last February, the National Institutes of Health and the Liberian government announced a clinical trial to study whether the American drug works.
Experience outside the study has been decidedly mixed. American aid works Brantly and Writebol were given Zmapp and survived. But a Liberian doctor and a Spanish priest who received the medication died.
The Zmapp study is still in progress, which Friede notes is a good sign, since studies get canceled if it becomes apparent the drug doesn’t work. “The fact that it hasn’t been stopped indicates there must be some signal of efficacy,” he said.
One potential problem with Zmapp is that it’s costly and time-consuming to produce.
GS-5734
This drug from Gilead, a California biopharmaceutical company, is so new it doesn’t even have a name yet. In animal studies, 100% of Ebola-infected monkeys who received the medicine survived, according to the company. In October, Gilead said they’d begun studies to determine if the drug is safe for humans.
BCX4413
This is another drug so new it doesn’t yet have a name. The National Institutes of Health is spending millions researching whether BCX4413 works against viruses like Ebola, according to BioCryst, the North Carolina company that makes the medicine. According to a company statement, the drug has had success fighting Ebola in non-human primates.
The also-rans
These three drugs have had mixed or unknown results, and experts seem pessimistic about their potential for treating Ebola:
Favipiravir
A study last year suggests this Japanese influenza drug might work against Ebola as long as patients have relatively low levels of the virus in their blood and are not terribly sick.
While the French sponsors of the drug trial were enthusiastic about the results, others said because of the way the trial was conducted, it’s still murky whether the drug works even for those with low viral loads.
“It resulted in that nebulous data zone that we were so fearful about,” said Dr. Luciana Borio, an official with the U.S. Food and Drug Administration, in the recent Science article. “We’re left with not knowing whether the product helps, hurts, or does nothing.”
Interferon
Canadian researchers have studied the use of this multiple sclerosis drug for Ebola but haven’t yet published the results. According to Friede, there were only nine patients in the study, so he said he doesn’t think the results will be meaningful.
Artesunate-amodiaquine
A recent study in the New England Journal of Medicine found that Ebola patients who took this anti-malarial drug had a lower risk of dying than those were took a different anti-malarial drug.
But experts are cautious for two reasons. One, the difference was not large: Those who took artesunate–amodiaquine were only 31% less likely to die than those who took the other drug, called artemether–lumefantrine. Two, the increased survival rate among those who took artesunate-amodiaquine might not be because the drug works — it might be because artemether–lumefantrine made Ebola patients more likely to die.
And then there’s Lamivudine
Interest in this HIV drug grew when CNN reported that at the height of the Ebola outbreak, a Liberian doctor, desperate to save his patients, began using it, which he had in plentiful supply in his hospital pharmacy. Dr. Gorbee Logan reasoned that the two viruses, Ebola and HIV, share some similarities in the way they replicate and spread throughout the body.
He told CNN in September of 2014 that he’d given the drug to 15 Ebola patients and all but two survived — this during a time when 70% of Ebola patients were dying in West Africa.
The world’s leading experts on Ebola dismissed Logan’s experience. About six weeks after CNN’s story, WHO issued a statement that “lamivudine has no antiviral activity against [Ebola] and should therefore not be administered for the treatment of Ebola.”
A few months later, the NIH published a letter in the journal Emerging Infectious Diseases reporting that because of CNN’s story they tried lamivudine in the lab, and it didn’t work.
CNN’s article about the Liberian doctor nevertheless piqued the interest of Stephen McCarthy, a graduate student in the department of laboratory medicine and pathobiology at the University of Toronto. Last spring, McCarthy tried lamivudine in the lab and found that it worked against the Ebola virus. Since he didn’t have access to one of the world’s few top-level biosafety labs, he had to use a toned-down version of the virus that wasn’t infectious and wouldn’t get humans sick.
Experts at the NIH and WHO were skeptical of McCarthy’s findings, since he didn’t use the actual Ebola virus but McCarthy was not deterred.
He and his supervisor, Donald Branch, managed to secure access to Canada’s BSL-4 lab, where infectious Ebola can be used. Their new study, published Monday in PLOS Neglected Tropical Diseases, suggests that lamivudine does work against Ebola in the laboratory.
Their study found the drug works even better when paired with another HIV medication, called AZT, or with interferon beta, used to treat multiple sclerosis. The combination of all three drugs was the most effective against Ebola.
The study was co-authored by Thomas Hoenen, an NIH virologist who specializes in hemorrhagic fever viruses such as Ebola, and by Gary Kobinger, a widely respected Ebola researcher who led the animal research on Zmapp.
But leaders at the WHO and NIH were unenthusiastic, because not only did lamivudine not work in the NIH’s lab, it also didn’t work when they gave it to 12 guinea pigs infected with Ebola. In science, as a general rule, animal studies trump lab studies, but the NIH researchers themselves called their animal work “a small pilot study.”
McCarthy said he still thinks lamivudine is worth further study, especially since it’s inexpensive, already available in Africa, and has been used safely for decades.
He added that as an HIV researcher, he doesn’t understand why authorities continue to study single drugs, rather than combinations. “The greatest success in HIV therapy is combination therapy. No one in HIV would give one drug,” he said.
But Hensley and Friede say in their opinion there’s no reason at this point to continue studying lamivudine. Friede puts lamivudine in the same category as countless other Ebola “remedies” that people latched onto during the horrific outbreak.
“If we should do further studies on lamivudine, then we should also have done them on homeopathy and snake venom and ozone injections,” he said.
A murky future
No cases of Ebola have been reported since November of last year, when a cluster of three cases arose in Liberia, according to the World Health Organization.
That’s obviously good news, but it also means there are nearly no patients to test the drugs on, so scientists have to rely on lab and animal studies. And they are inferior substitutes. Treatments that work on cells in laboratories (in vitro studies) don’t always work in animals (in vivo studies), and those that work in animals don’t always work in people.
“It’s important to stress that one of the challenges for the research scientists is understanding what the various in vitro and in vivo screens mean,” Lisa Hensley, a top NIH Ebola researcher wrote to CNN in an email.
Dr. Donald Thea, director of the Center for Global Health and Development at the Boston University School of Public Health, agrees. Without human study subjects, he said, you can only go so far.
“It absolutely limits you as to how close you can get to a home run without humans,” he said. The trick, he said, is to be ready to hit the ground running with strong potential drug candidates if and when another large Ebola outbreak occurs — and it’s not clear if such candidates currently exist.