Penn State researchers develop test prototype that delivers results in 45 minutes
UNIVERSITY PARK, Pa. — PCR tests, also called molecular tests or nucleic acid tests, are considered the gold standard in detecting the presence of SARS-CoV-2, the virus that gives rise to COVID-19.
However, they can take a few days to process, resulting in unnecessary quarantine for negative individuals or delays for those who require proof of negative testing for travel or other commitments.
Rapid antigen-detecting tests, on the other hand, are convenient, but less reliable than PCR tests.
To bridge the gap between accuracy and convenience, Penn State researchers have developed an at-home, saliva-based testing platform that can provide results in 45 minutes.
In preliminary tests, the platform detected the COVID-causing virus with the same level of sensitivity as PCR tests. Their results published in ACS Sensors.
“PCR test results take about an hour to develop in a lab, but you have to factor in the time it takes to send the sample to a lab and for the lab to process it,” said principal investigator Weihua Guan, associate professor of electrical engineering and of biomedical engineering in Penn State’s College of Engineering.
“We wanted to create a viable alternative to the PCR for people to use at home, without having to endure the invasive nasal test.”
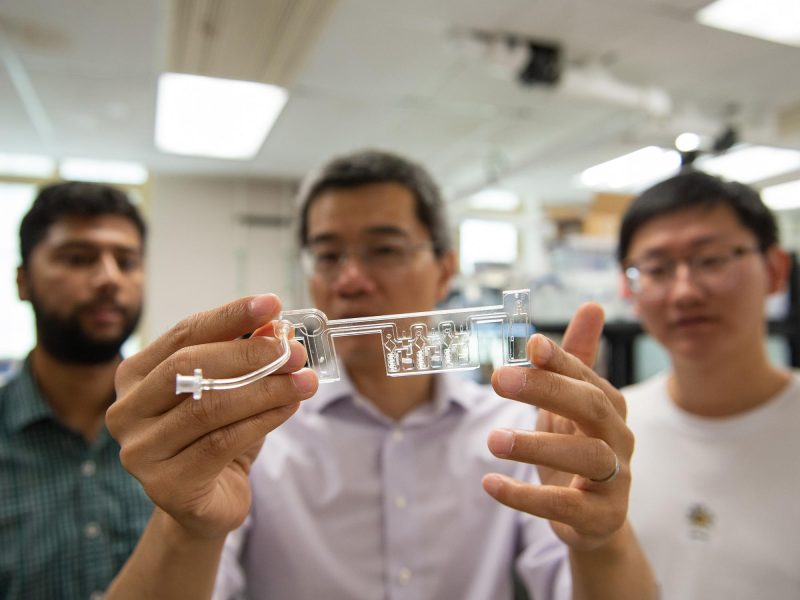
Guan and his team developed a palm-sized testing kit, where an individual spits into a cartridge and inserts it into processing platform. Within 45 minutes, test results are sent to a custom android app developed by the researchers.
The platform uses reverse transcription loop-mediated isothermal amplification, or RT-LAMP, to detect the virus.
The testing device first heats the saliva to 203 degrees Fahrenheit, the temperature at which viral particle shells break apart and release their genetic material.
The genetic material is then mixed with pre-packaged reagents in a microfluidic cartridge. Finally, the sample is cooled to 149 degrees Fahrenheit, triggering another chemical reaction in which a few viral molecules are multiplied into billions of copies, making the virus easier to identify.
If the virus is present in the saliva sample, the user will receive a positive result on their connected smartphone app.
To test the setup, Guan and his team infused human saliva samples purchased commercially with inactivated SARS-CoV-2 virus particles and ran the samples through the prototype.
They also tested a couple of clinical specimens. The platform accurately determined whether every sample was positive or negative for the virus.
“We tested hundreds of mock samples and controlled the quantity of COVID particles in each one,” Guan said. “Our platform proved to be highly sensitive to the presence of the virus in both the mock and clinical samples, with the standards set by the PCR test as our benchmark.”
The researchers said they plan to continue testing their platform with more clinical COVID samples through a collaboration with Yusheng Zhu, medical director of the Clinical Chemistry and Automated Testing Laboratory at the Penn State Milton S. Hershey Medical Center.
In addition to more clinical testing, the researchers also are working to improve the test’s short shelf life, as the enzymes in the prototype degrade at room temperature within three days of production. The team is experimenting with reagent lyophilization, a method of freeze-drying biological material that can extend enzyme shelf life. According to Guan, preliminary results indicate the method will allow the RT-LAMP test to last at least six months at room temperature in stores or in the medicine cabinet at home.
The researchers filed a provisional patent application on their device and said they plan to commercialize it, pending scaled-up clinical testing and review by the U.S. Food and Drug Administration.
Suresh V. Kuchipudi, interim director of Penn State’s Animal Diagnostic Laboratory (ADL) and Dorothy Foehr Huck and J. Lloyd Huck Chair in Emerging Infectious Diseases, and Michele Yon, research technologist with ADL, acquired the clinical samples tested in this work. Other contributors include Zifan Tang, Aneesh Kshirsagar and Tianyi Liu, all Penn State doctoral students in electrical engineering, and Jiarui Cui, a Penn State undergraduate student in electrical engineering.
The National Institutes of Health, the National Science?Foundation and the Penn State Coronavirus Research Seed Fund supported this work.